Meniscus Tear MRI: Your Guide To Understanding Knee Scans
A torn meniscus is a common knee injury that affects the cartilage which acts as a cushion between the bones of the knee. It can cause pain, swelling, and difficulty in moving the knee, significantly impacting daily life and mobility. Understanding the nature of this injury is the first step towards effective treatment, and for that, a Magnetic Resonance Imaging (MRI) scan is indispensable.
Magnetic Resonance Imaging (MRI) is a highly effective tool used to diagnose a torn meniscus. This advanced imaging technique provides clear, detailed pictures of the internal structures of the knee, which helps in accurately identifying the presence, type, and extent of a meniscal tear. Understanding its implications is vital for determining appropriate treatment strategies to restore mobility and alleviate pain.
Table of Contents
- Understanding the Menisci: The Knee's Essential Cushions
- Why Meniscal Tears Occur: Acute vs. Chronic
- The Unrivaled Role of MRI in Diagnosing Meniscus Tears
- Decoding Your Meniscus Tear MRI Scan: What Radiologists Look For
- Navigating the Nuances: Avoiding Diagnostic Pitfalls in Meniscus Tear MRI
- Beyond Direct Signs: Indirect Clues on Your Meniscus Tear MRI
- Evolving Insights: New Discoveries in Meniscus Anatomy and Tears
- The Impact of a Meniscus Tear Diagnosis: What Comes Next
Understanding the Menisci: The Knee's Essential Cushions
Before delving into the specifics of a meniscus tear MRI, it's crucial to understand what the menisci are and why they are so important. Menisci are small fibrocartilaginous structures that are essential for knee stability and the preservation of articular cartilage. Located between the thigh bone (femur) and the shin bone (tibia), each knee has two menisci: the medial meniscus (on the inner side of the knee) and the lateral meniscus (on the outer side). These crescent-shaped cartilages act as shock absorbers, distributing weight evenly across the knee joint and providing stability during movement. They also play a role in joint lubrication and nutrition, contributing significantly to the overall health and longevity of the knee joint. Without healthy menisci, the knee joint is more susceptible to wear and tear, leading to conditions like osteoarthritis. This article discusses the anatomy and function, variations, appearance and consequence of tears, and postoperative evaluation, setting the stage for understanding why their integrity is so vital and how a meniscus tear MRI helps in assessing their condition.
Why Meniscal Tears Occur: Acute vs. Chronic
Meniscal tears are the failure of the fibrocartilaginous menisci of the knee. They represent one of the most common knee injuries, affecting people of all ages, from athletes to older adults. These tears can occur in an acute or chronic setting, each with distinct mechanisms and implications. Acute meniscal tears typically occur after a sudden rotational movement of the knee, often when the foot is planted and the body twists. This twisting motion, common in sports like soccer, basketball, and skiing, can trap the meniscus between the femur and tibia, leading to a tear. Pathology acute meniscal tears often involve significant force and can be quite painful, sometimes accompanied by a popping sensation at the time of injury. The immediate aftermath usually involves swelling, pain, and difficulty in bending or straightening the knee. In contrast, chronic meniscal tears often develop gradually over time due to degenerative changes in the meniscus. As we age, the meniscus can become less elastic and more brittle, making it susceptible to tearing even with minor trauma or everyday activities like squatting or kneeling. These degenerative tears may not have a distinct injury event and can present with intermittent pain, stiffness, and swelling that worsens over time. Understanding the context of the tear—whether acute or chronic—is important for clinical assessment and treatment planning, though the ultimate diagnostic precision often rests with a meniscus tear MRI.
The Unrivaled Role of MRI in Diagnosing Meniscus Tears
When it comes to diagnosing meniscal tears, Magnetic Resonance Imaging (MRI) continues to be the imaging modality of choice. Its ability to provide detailed images of soft tissues, including cartilage, ligaments, and tendons, makes it superior to X-rays, which primarily show bone. MRI is crucial in diagnosing these tears, offering detailed images that reveal the extent and configuration of the injury. The precision of a meniscus tear MRI is well-documented, with sensitivity and specificity for diagnosing meniscus tears being as high as 93% and 88%, respectively [15]. This high level of accuracy means that MRI is not only excellent at detecting the presence of a tear but also at ruling one out. It's the best imaging study to detect a torn meniscus because it uses a strong magnetic field to produce detailed images of both hard and soft tissues within your knee. This allows clinicians to visualize the menisci in multiple planes, providing a comprehensive view that is essential for accurate diagnosis and subsequent treatment planning. While clinical examination can suggest a meniscal tear, a meniscus tear MRI provides the definitive evidence needed to confirm the diagnosis, understand the specific type of tear, and guide surgical or non-surgical interventions. Meniscal tears are best evaluated with MRI due to its non-invasive nature and unparalleled detail.
Decoding Your Meniscus Tear MRI Scan: What Radiologists Look For
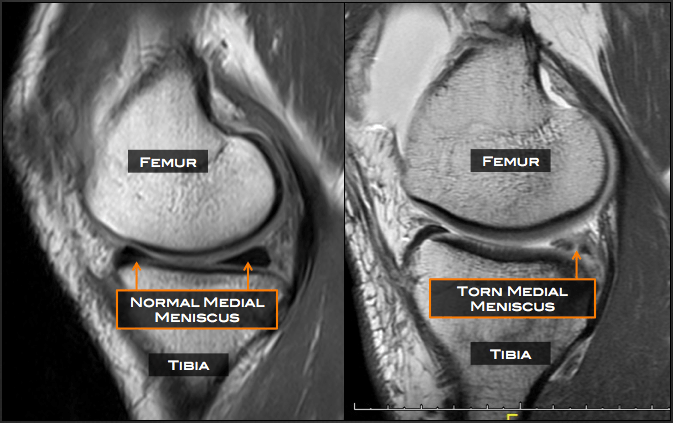
Interpreting a meniscus tear MRI scan requires specialized knowledge, but understanding the basic principles can help patients grasp their diagnosis. On MRI, meniscal tears are usually diagnosed as a linear signal intensity that extends from meniscal substance to a free edge (figure 1). This "linear signal" represents fluid within the tear, which lights up brightly on certain MRI sequences. Identification of meniscal tears has long been based on two primary criteria: first, intrameniscal signal intensity exiting the superior or inferior articular surface of the meniscus on short TE sequences, and second, the presence of a clear line of signal extending to the articular surface. These are the fundamental visual cues that radiologists look for. Christopher Centeno, a renowned expert, describes how to read a knee MRI for meniscal tear and what it means to have a meniscus tear vs. a normal meniscus, emphasizing the importance of recognizing these specific signal patterns. Learning how to read an MRI scan for a meniscus tear involves recognizing these key imaging features and understanding their clinical significance. Discovering these key imaging features, common tear patterns, and tips to interpret knee MRI results is essential for both diagnosing clinicians and informed patients.
Key Imaging Features and Diagnostic Criteria
When a radiologist examines a meniscus tear MRI, they are looking for specific changes in the signal intensity and morphology of the menisci. As mentioned, the hallmark sign is a linear signal intensity that clearly extends to the articular surface of the meniscus. This means the tear has created a path for fluid to enter the meniscal substance, which is then picked up by the MRI scanner. The specific MRI sequences, particularly those with short echo times (TE), are optimized to highlight this fluid signal. Beyond this primary criterion, radiologists also assess the location, orientation, and extent of the tear. For instance, a tear might be located in the anterior horn, body, or posterior horn of the meniscus. Its orientation could be horizontal, vertical, radial, or complex. The extent refers to whether it's a partial or complete tear. The presence of associated findings, such as bone bruising or fluid collections, also provides additional clues about the nature and severity of the injury. A thorough understanding of normal meniscal anatomy and its variations is paramount, as certain normal structures or degenerative changes can sometimes mimic a true tear, making the interpretation of a meniscus tear MRI a nuanced skill.
Common Tear Patterns and Their Significance
Meniscal tears come in various patterns, each with distinct implications for treatment and prognosis. Two common patterns highlighted in the provided data are horizontal cleavage tears and radial tears. Learning how to identify a horizontal cleavage tear in the medial meniscus from different MRI views is crucial for accurate diagnosis. This type of tear typically runs parallel to the tibial plateau, essentially splitting the meniscus into upper and lower halves. They are often associated with degenerative processes and can sometimes lead to the formation of a parameniscal cyst. Watch a video by Minnesota knee surgeon Dr. Robert LaPrade, who explains the specifics and shows examples of the tear pattern, emphasizing the importance of recognizing these distinct configurations. Another significant pattern is the radial tear, particularly of the lateral meniscus. An axial view MRI scan demonstrating a complete radial tear of the lateral meniscus shows the meniscus essentially sliced in two, and the edges tend to pull apart. These tears are particularly ominous because they disrupt the circumferential fibers of the meniscus, which are vital for its hoop stress function and load-bearing capacity. If the patient is young and/or if there is fairly normal cartilage present, lateral meniscus radial tears should have an attempt at a repair, as the success rate in a systematic review was approximately 80-90%. Understanding these common tear patterns on a meniscus tear MRI is vital for guiding surgical decisions, as some tears are more amenable to repair than others.
Navigating the Nuances: Avoiding Diagnostic Pitfalls in Meniscus Tear MRI
While MRI is a highly accurate imaging method for diagnosing meniscal tears, its interpretation is not without challenges. To avoid errors in diagnosing meniscal tears, those interpreting MR examinations of the knee need to be aware of the attachments of the menisci and the normal variations in meniscal anatomy that may resemble a meniscal tear. For instance, certain meniscal ligaments or vascular channels can sometimes appear as linear signals within the meniscus, leading to a false-positive diagnosis if not properly recognized. Similarly, the normal aging process can lead to degenerative changes within the meniscus that manifest as increased signal intensity, but without extending to the articular surface, these are not true tears. Awareness of common diagnostic errors can ensure accurate diagnosis of meniscal tears. This includes understanding artifacts that can occur during the MRI scan itself, which might obscure or mimic pathology. In addition, by being aware of the patterns of meniscal tears, it is easier to diagnose complex or atypical presentations. Radiologists and clinicians must possess a deep understanding of both normal and pathological knee anatomy, coupled with extensive experience in MRI interpretation, to confidently differentiate a true meniscus tear from other findings. We also address pitfalls and signs which can help improve diagnostic accuracy, underscoring the continuous learning required in this field.
Beyond Direct Signs: Indirect Clues on Your Meniscus Tear MRI
Occasionally, meniscal tears can be difficult to detect at imaging, even with the high resolution of a meniscus tear MRI. This can happen with very small tears, tears in unusual locations, or tears that are obscured by other pathology. In such cases, radiologists rely on secondary indirect signs that, while not direct evidence of a tear, should significantly increase the radiologist’s suspicion for an underlying tear. These indirect signs are subtle clues that point towards a meniscal injury, even if the tear itself is not clearly visualized. One such sign is a parameniscal cyst, which is a fluid collection adjacent to the meniscus. These cysts often form when synovial fluid leaks out through a meniscal tear, acting as a "pop-off valve" for the intra-articular pressure. Another important indirect sign is meniscal extrusion, where the meniscus is displaced outwards from the joint space. This often indicates a significant tear that compromises the meniscal root or peripheral attachments, allowing the meniscus to be pushed out from its normal position. Linear subchondral bone marrow edema, which is swelling within the bone directly beneath the cartilage, can also be an indirect sign. This edema suggests increased stress or impact on the bone, often as a result of the meniscus no longer effectively cushioning the joint. The presence of one or more of these secondary signs on a meniscus tear MRI should prompt a more thorough search for a subtle tear or a consideration for further imaging or clinical correlation.
Evolving Insights: New Discoveries in Meniscus Anatomy and Tears
The field of knee imaging, particularly regarding the menisci, is constantly evolving. While there are decades of MRI literature on the tears involving the meniscus body and horns, there is now a surge in knowledge regarding injuries at the meniscus roots and periphery. Meniscal root tears, for example, are increasingly recognized as significant injuries that can lead to rapid degenerative changes in the knee, as they effectively detach the meniscus from its bony anchor, compromising its ability to distribute load. These tears were historically often missed or underestimated but are now a major focus due to their profound impact on knee biomechanics and long-term joint health. The authors briefly highlight new insights into meniscus anatomy and then summarize recent developments in the understanding of these complex injuries. This includes a deeper appreciation for the intricate attachments of the menisci to the surrounding capsule and ligaments, and how injuries to these peripheral regions can affect overall knee stability. Advanced MRI techniques and sequences are also continually being developed to better visualize these subtle but critical tears. This ongoing research and improved understanding mean that the interpretation of a meniscus tear MRI is becoming even more precise, allowing for earlier and more targeted interventions that can potentially prevent or slow the progression of osteoarthritis in the knee.
The Impact of a Meniscus Tear Diagnosis: What Comes Next
Receiving a diagnosis of a meniscus tear, confirmed by a detailed meniscus tear MRI, is a critical step, but it's just the beginning of the journey towards recovery. Understanding its implications is vital for determining appropriate treatment strategies to restore mobility and alleviate pain. The treatment approach for a torn meniscus varies widely depending on several factors, including the type, size, and location of the tear, the patient's age, activity level, and overall knee health. Some tears, particularly small, stable ones in the outer, vascularized part of the meniscus, may heal with conservative management, involving rest, ice, compression, elevation (RICE), physical therapy, and pain medication. However, many tears, especially larger or more complex ones, or those causing persistent symptoms, may require surgical intervention. Surgical options typically include meniscal repair, where the torn edges are stitched back together, or partial meniscectomy, where the damaged portion of the meniscus is removed. The goal of any treatment is to restore the knee's function, reduce pain, and ideally, preserve as much of the meniscal tissue as possible to protect the articular cartilage from future damage. Postoperative evaluation, often involving follow-up MRI scans, is crucial to monitor healing and ensure the success of the intervention. The detailed information provided by the initial meniscus tear MRI guides these crucial decisions, making it an indispensable tool in modern orthopedic care.
In conclusion, the meniscus tear MRI stands as an indispensable diagnostic tool in the realm of knee injuries. Its unparalleled ability to visualize the intricate soft tissues of the knee provides critical information regarding the presence, type, and extent of meniscal tears, guiding both conservative and surgical treatment pathways. While interpretation requires expertise and an awareness of potential pitfalls and anatomical variations, the continuous evolution of MRI technology and our understanding of meniscal pathology only enhances its accuracy. From identifying common tear patterns like horizontal cleavage and radial tears to recognizing subtle indirect signs, the detailed insights from a meniscus tear MRI are vital for restoring mobility and alleviating pain for countless individuals. If you're experiencing knee pain or suspect a meniscal injury, always consult with a qualified healthcare professional who can accurately diagnose your condition and recommend the most appropriate course of action, often beginning with this pivotal imaging study. Share this article to help others understand the importance of MRI in knee health, and explore more of our resources on musculoskeletal health.


Detail Author:
- Name : Laron Murray
- Username : frederique01
- Email : gisselle.mills@gusikowski.com
- Birthdate : 1971-12-28
- Address : 191 Jerde Villages Apt. 554 Damionbury, MS 65685
- Phone : +1.726.267.3023
- Company : Ullrich Ltd
- Job : Administrative Services Manager
- Bio : Iste saepe voluptatibus aliquam sunt ipsum pariatur eos nemo. Aut sit et eos officiis quia distinctio. Aut odit incidunt explicabo officiis et laudantium cumque.
Socials
twitter:
- url : https://twitter.com/lehners
- username : lehners
- bio : Delectus est sit exercitationem ut error et. Laboriosam quae voluptatum autem ratione illum sed sit. Numquam atque blanditiis sed.
- followers : 1598
- following : 346
tiktok:
- url : https://tiktok.com/@sabina6570
- username : sabina6570
- bio : Non qui minus cumque. Vitae possimus dolore qui aliquam aut.
- followers : 3460
- following : 455
instagram:
- url : https://instagram.com/sabina.lehner
- username : sabina.lehner
- bio : Culpa eos ad ut ad. Vitae ut aut laudantium numquam. Atque corrupti dicta ut alias.
- followers : 759
- following : 1380
facebook:
- url : https://facebook.com/slehner
- username : slehner
- bio : Eos odit eos facere pariatur quam consequatur cumque dignissimos.
- followers : 3747
- following : 2442
linkedin:
- url : https://linkedin.com/in/slehner
- username : slehner
- bio : Harum voluptatum tempore modi.
- followers : 3755
- following : 742